News
A new breakthrough in cancer treatment
Neutralising GDF-15 may provide a highly promising therapeutic approach for patients suffering from certain types of cancer such as melanoma

An international team of researchers, including Prof. Michel Mittelbronn, Head of the National Centre of Pathology at the Laboratoire Nationale de Sante and the Luxembourg Centre of Neuropathology at the Luxembourg Institute of Health (LIH), has uncovered a key defence mechanism in certain tumours that makes them resistant to treatment. Thanks to such advances, current immunotherapies will have a much higher chance of success. A better understanding of how malignant cells protect themselves is essential to effectively combat cancer.
Cancer cells and the GDF-15 cytokine
In their recently published paper in the journal Nature Communications (see Nat Commun. 2023 14 :4253), the researchers were able to demonstrate how cancer cells block access to our immune system. “A malignant tumour is a foreign entity that our body is normally able to identify and destroy. We carry cancer cells inside of our bodies all the time, but our immune system takes care of them”, explains Prof. Mittelbronn, who also leads a research team at the University’s Luxembourg Centre for Systems Biomedicine. “The GDF-15 cytokine, however, inactivates this immune response.”
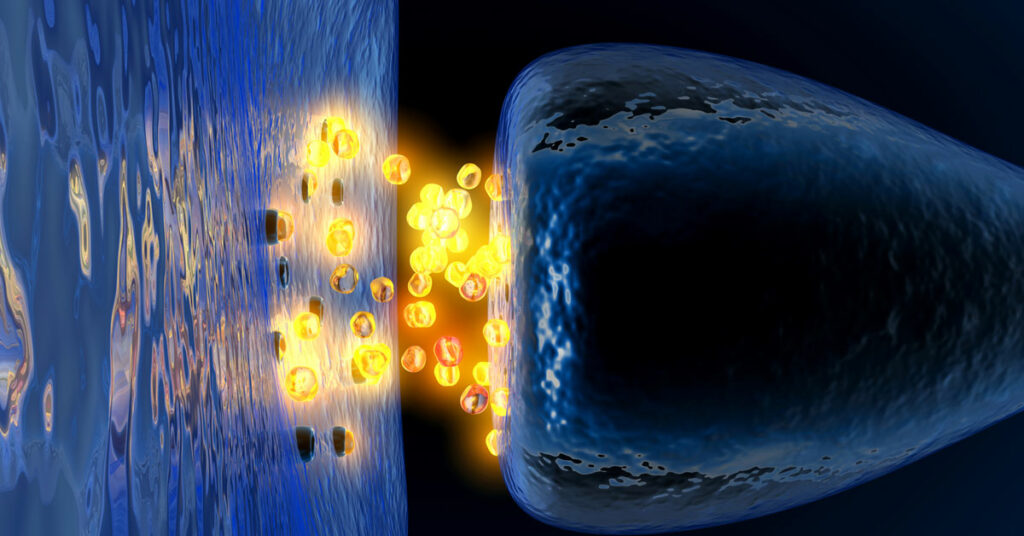
With the help of mouse models, in vitro pharmacological studies and analyses of melanoma patients, the researchers were able to determine how GDF-15 works. This protein is abundantly secreted by solid tumours such as those found in melanoma, liver cancer and bladder cancer. It stops our immune system’s infantry – the famous T lymphocytes – from infiltrating the lesion. T lymphocytes are transported by the bloodstream. For them to exit and attack the tumour, they must first attach themselves to the walls of the blood vessels at the right point. GDF-15 prevents this. In other words, our troops are missing their stop because the enemy has demolished the road signs.
Due to GDF-15, the few soldiers that do manage to reach their goal will additionally find themselves in a state of irreparable exhaustion, utterly unable to do their job.
There is a highly significant negative correlation between GDF-15 expression and the number of T lymphocytes present in the tumour environment. Furthermore, the survival curves are quite striking: patients with a high level of GDF-15 die significantly earlier
says Prof. Mittelbronn.
How can this new knowledge about GDF-15 be used to improve immunotherapy?
PD-1 (for Programmed cell Death protein) is a protein present on the surface of T lymphocytes that interacts with another protein called PD-L1 (L for Ligand), present on the surface of tumour cells. This interaction is far from beneficial. PD-L1 mimics what is known as an immune checkpoint, a sort of cellular ID card preventing T lymphocytes from attacking non-cancerous cells. By creating this false identity, cancer cells disable T lymphocytes.
The aim of current anti-PD1/anti-PD-L1 immunotherapy is to prevent this from happening. However, as long as GDF-15 is produced, there is little hope of success as the T lymphocytes do not even reach their destination and, even if they do, they are rendered useless. Given that GDF-15 is highly over-expressed in around 50% of solid human tumours, blocking it could have a significant impact on the efficiency of immunotherapy.
As for potential side-effects, Prof. Mittelbronn explains: “This type of therapy could provoke autoimmune reactions by activating our immune system but clinical studies will tell us more. It will be essential to select patients carefully. Anti-GDF-15 therapy is suitable only for those patients with a high level of cytokine over-expression in the tumour environment.”
Can the activation of T lymphocytes cure all types of cancer?
“It depends,” explains Prof. Mittelbronn. “Brain tumours, for example, are not very immunogenic, which means that the immune system does not necessarily recognise them as a threat and the T-cell response plays a minor role in such cases. Melanomas, on the other hand, generate a high immune response due to exposure to the sun, which causes extensive DNA damage and cell mutations. They are often eliminated before we even realise it. The role played by T lymphocytes in these types of cancers is therefore crucial and the response to anti-GDF-15 therapy could be sensational.”